Author: sajimone
-
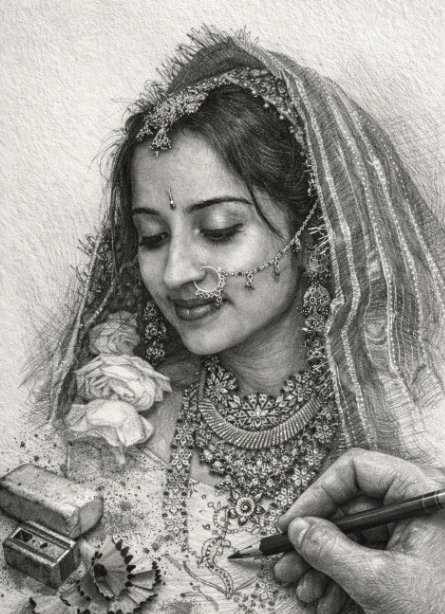
A Diamond Forged Through Fire
A birthday tribute to three decades of growing up together I met Nidhi when I was eighteen and thought I knew everything. She was nineteen and my resident assistant at the University of South Florida, already carrying losses that would have broken most people twice her age. Her father passed the previous year. Her twin…
-
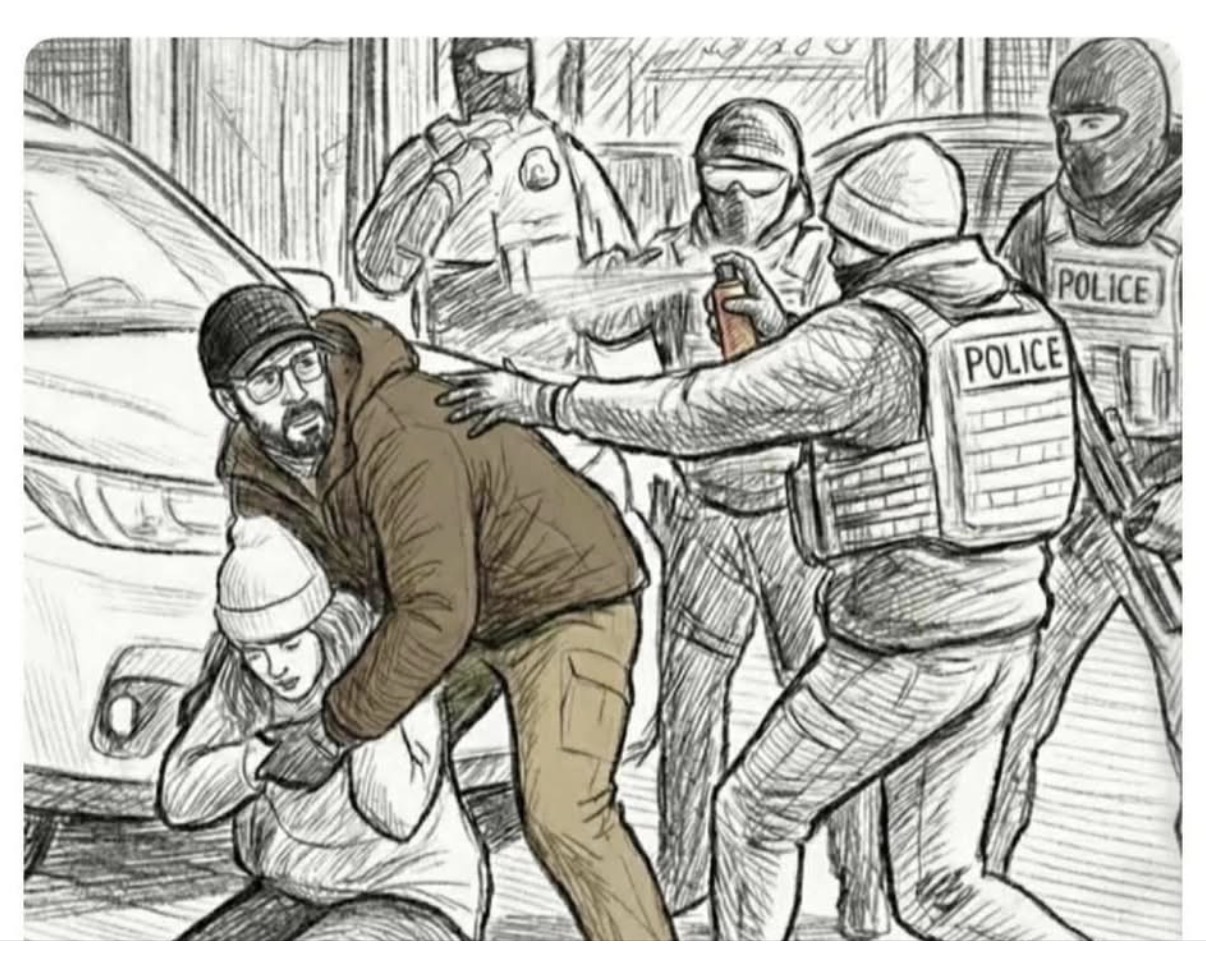
This Is My Protest: A Call for Moral Reckoning
Another American has died—shot down in the street. A U.S. citizen. An ICU nurse. A helper. A human being. When I watch the video of what happened to Alex Pretti, what really strikes me isn’t just the senselessness of it — it’s how ordinary and humane his actions appeared in that moment. Alex wasn’t running…
-

Why I Got Into Real Estate (Even as a Devoted Oncologist)
Reflections on identity, burnout, financial freedom — and the horror stories that taught me resilience Recently, I was at a casual get‑together when a friend asked me an interesting question: “You’re an oncologist — you help patients every day. Why real estate? Is that the right thing to do with your time?” At first, I…
-

4Ever Young Winter Garden Soft Opening
I’m excited to share that our first 4Ever Young location—the first of three—is opening soon in Winter Garden, and we’re officially in the final stages of our build-out. Seeing this space come together and watching the full team and vendors fall into place has been incredibly rewarding. We’ll be hosting a soft opening for friends…
-

Letting Go, One Step at a Time
This weekend, we drove our daughter Simran to Gainesville to begin her college journey at the University of Florida. It was bittersweet. On one hand, it’s deeply fulfilling to watch your child grow into a young lady—to see her step forward with confidence, curiosity, and independence. On the other hand, it’s impossible not to feel…
-

Reflecting on 2025 and Looking Ahead to 2026: Milestones, Gratitude, and New Beginnings
As we close out 2025, I find myself pausing to reflect on what has been an extraordinary year—one marked by significant financial milestones, professional transitions, personal growth, and precious time with family. I’m writing this from Europe, Bologna Italy to be exact, where my family and I are spending the final two weeks of the…
-

Every Sunday Morning Might Be the Last
Yesterday morning, I played basketball for the first time in over a month—coming off yet another knee injury in what’s been a year of on-and-off playing. We ran for almost two hours, and by the end, I was completely wiped out—physically useless until this Monday morning. But as drained as I felt, I also felt…
-

Now Hiring: General Manager for Our First 4Ever Young Wellness & Aesthetic Center in Winter Garden Florida
We’re thrilled to announce that we’re halfway through the build-out phase of our first 4Ever Young location in Winter Garden, FL, and it’s time to take the next big step: hiring our founding team. This is the first of three planned locations, and it’s more than just a business—this is a mission-driven venture to help…
-

The Third Space: Finding Balance Between Work, Home, and Spirituality
Just a quick update before diving in: I’ll be starting at AdventHealth on December 1st, 2025, and I’m really looking forward to this next chapter. If you’ve noticed a lull in posts lately, it’s because I’ve been buried in board review—studying for my hematology recertification—while also ramping up with my wife on our first franchise…
-
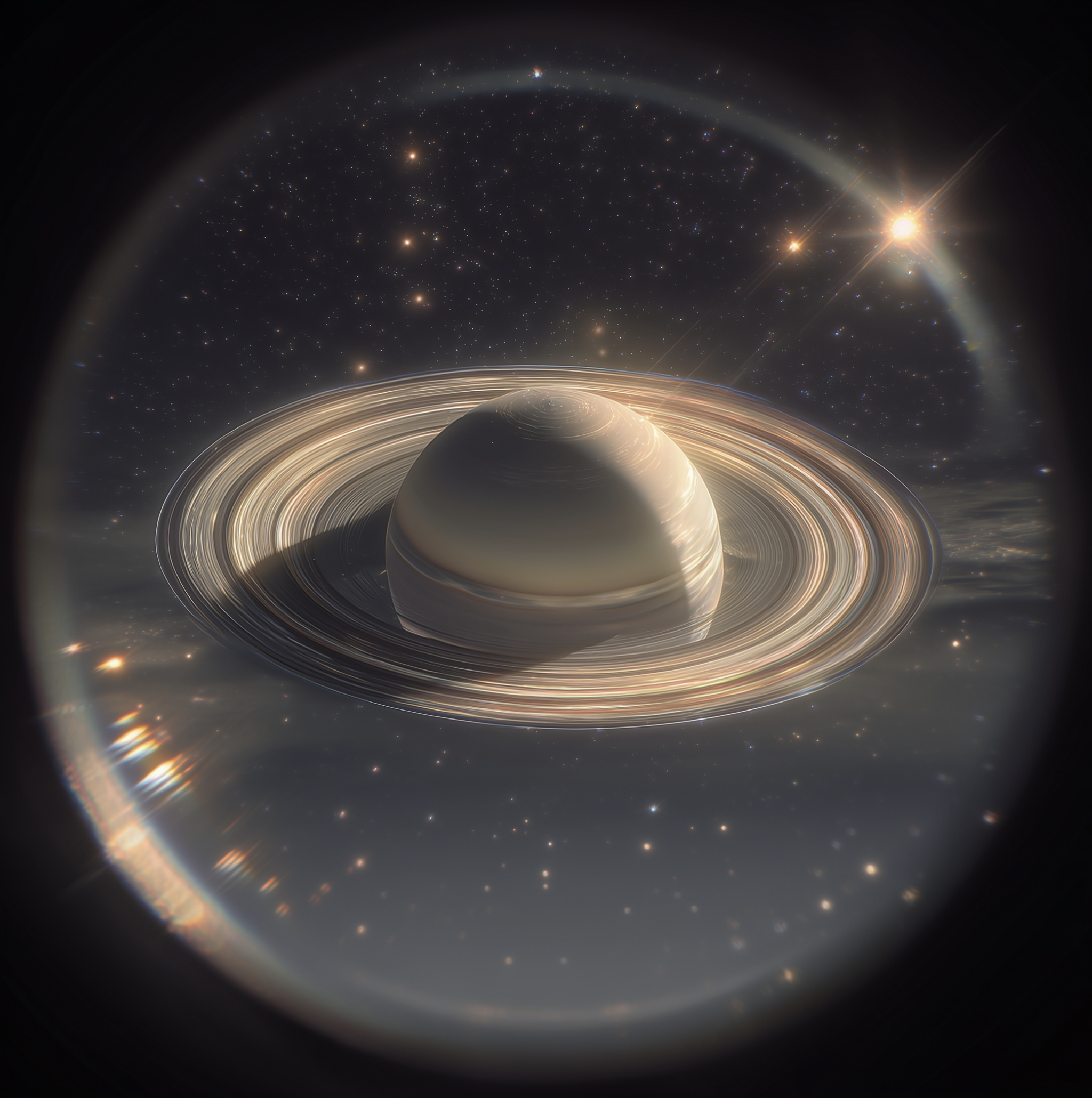
This is “Hocking” Hard: 22,000 Steps, the Value of Struggle and Saturn
One of the unexpected gifts of doing locums work is the chance to explore corners of the country I might never have otherwise visited. Recently, I had the chance to spend a weekend with my family in Columbus, Ohio and just south of it, in the hidden gem of Hocking Hills State Park. Columbus itself is…